Raised PSA
Prostate Cancer
Prostate cancer has become the most common cancer in men and is the second most common cause of male cancer deaths, after lung cancer. It is different from most cancers in that a significant proportion of men, particularly older men with a shorter life expectancy, have a very slow growing form of this cancer, meaning that it is unlikely to cause symptoms or progress beyond the prostate gland during their lifetime. Sometimes in younger men the cancer can be small, slow growing and present only a limited risk to the patient. Clinically important prostate cancers can be defined as those that threaten the well-being or life span of a man.
What are the sympptoms of prostate cancer?
Often prostate cancer does not produce any symptoms, or it may produce symptoms similar to benign enlargement of the prostate, BPH. These include:
- difficulty in starting to pass urine
- poor flow of the urinary stream
- dribbling at the end of the stream
- the feeling the need to pass urine frequently, including at night,
- an urgent need to rush to pass urine, occasionally without any warning
- passing blood in urine
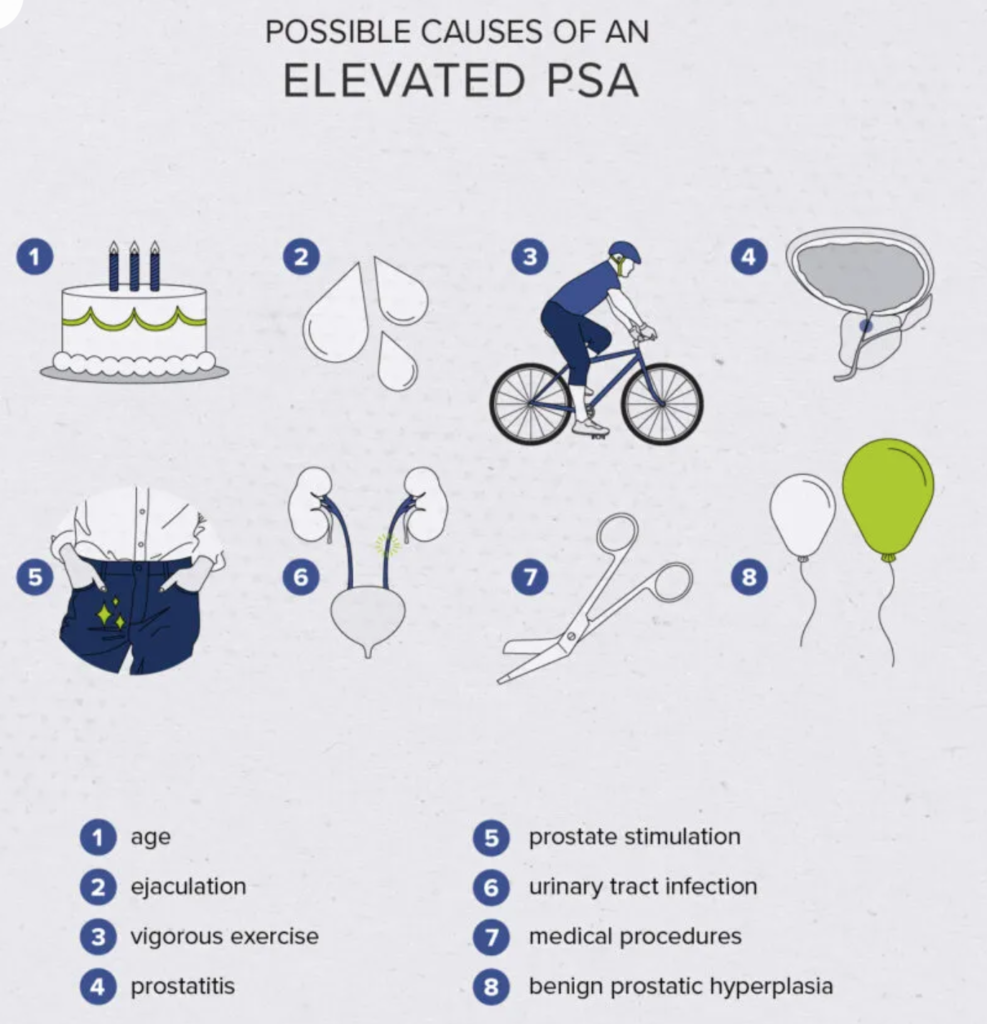
Often patients are diagnosed with prostate cancer after they are found to have a raised PSA blood test, or because they have an abnormal feeling prostate. However, PSA test is not entirely accurate. There is no real safe lower limit. Even in men with “normal” levels of PSA (less than 3 to 4 ng/ml depending on your age) around 15% may have small prostate cancers. Conversely, the PSA level may be increased by conditions other than the presence prostate cancer, such as BPH, urinary tract infection or prostatitis (infection in the prostate).
How is prostate cancer diagnosed.
If the tumour in the prostate is large enough to be felt, your doctor may be able to examine it. With a gloved and lubricated finger, your doctor feels the prostate and surrounding tissues from the rectum. Hard or lumpy areas may suggest the presence of one or more tumours. Your doctor may also be able to tell whether it’s likely that the tumour has grown outside the prostate.
Men will almost always need to undergo an MRI and a transrectal prostate biopsy or a transperineal prostate biopsy in order to establish the diagnosis of prostate cancer.
Magnetic resonance Imaging
A multi-parametric MR imaging test (mp-MRI) has been shown to identify areas in the prostate suspicious for cancer. Mp-MRI uses 2-3 sophisticated interpretations of digital information from the scan to allow the radiologist to identify these abnormality. It is now known that the accuracy of MRI is superior to any laboratory test available so far. Although the quality is outstanding, mp-MRI cannot diagnose prostate cancer alone and it also cannot fully exclude prostate cancer either. A biopsy is most commonly still required. However, it can give valuable information regarding the risk of prostate cancer, if it is normal, and suspicious areas can be targeted using MRI-US fusion technology. Paimaun Zakikhani works closely with the Radiologists at Prostate Care who are accredited experts in reading Prostate mp-MRI.


Prostate biopsy
Prostate biopsy involves taking several cores of prostate tissue using an ultrasound probe placed in the rectum, and is usually done under local anaesthetic. On some occasions, a transperineal template or prostate mapping biopsy may be appropriate. This involves a general anaesthetic, the biopsies are taken through the soft skin underneath the scrotum and above the anus.
What is the Gleason Score
The prostate tissue that was removed during the biopsy procedure can be used in lab tests. The pathologist studies prostate tissue samples under a microscope to determine the grade of the tumour. The grade tells how different the tumour tissue is from normal prostate tissue.
Tumours with higher grades tend to grow faster than those with lower grades. They are also more likely to spread. Doctors use tumour grade along with your age, overall health and other factors to suggest treatment options. The most commonly used system for grading prostate cancer is the Gleason score. Gleason scores range from 6 to 10.
To come up with the Gleason score, the pathologist looks at the patterns of cells in the prostate tissue samples. The most common pattern of cells is given a grade of 1 (most like normal prostate tissue) to 5 (most abnormal). If there is a second most common pattern, the pathologist gives it a grade of 1 to 5 and then adds the grades for the two most common patterns together to make the Gleason score (e.g.3 + 4 = 7). If only one pattern is seen, the pathologist counts it twice (5 + 5 = 10).
A high Gleason score (such as 10) means a high-grade prostate tumor. High-grade tumors are more likely than low-grade tumors to grow quickly and spread.
Treatment options
Men with prostate cancer have many treatment options. Treatment options include:
- Active Surveillance
- Surgery
- Radiation therapy
- Hormone therapy
You may receive more than one type of treatment. The treatment that’s optimal for one man may not be optimal for another. The treatment that’s right for you depends mainly on:
- Your age
- Gleason score (grade) of the tumour
- Stage of prostate cancer
- Your symptoms
- Your general health
